Find your ACA confidence
Navigate reporting and regulatory complexities with tools that bring clarity to compliance

Trusted by over 3,000 providers





Is your HR & payroll system built for healthcare?
Complexities of ACA call for an ally, let us be that ally
Compliance confidence
Know your compliance status with precision tools that work
Reporting made clear
Generate and file ACA forms accurately without the hassle
More time for what matters
Reduce admin burden with efficient, automated workflows
Guidance that counts
Access experts who know healthcare compliance inside and out
ACA tools integrated for your team
Link ACA compliance with payroll, benefits, and HR solutions in one seamless platform bringing clarity to complex requirements
Compliance without compromise
Features
Determine eligibility status
Track full and part-time status for each employee to ensure accurate ACA reporting and compliance
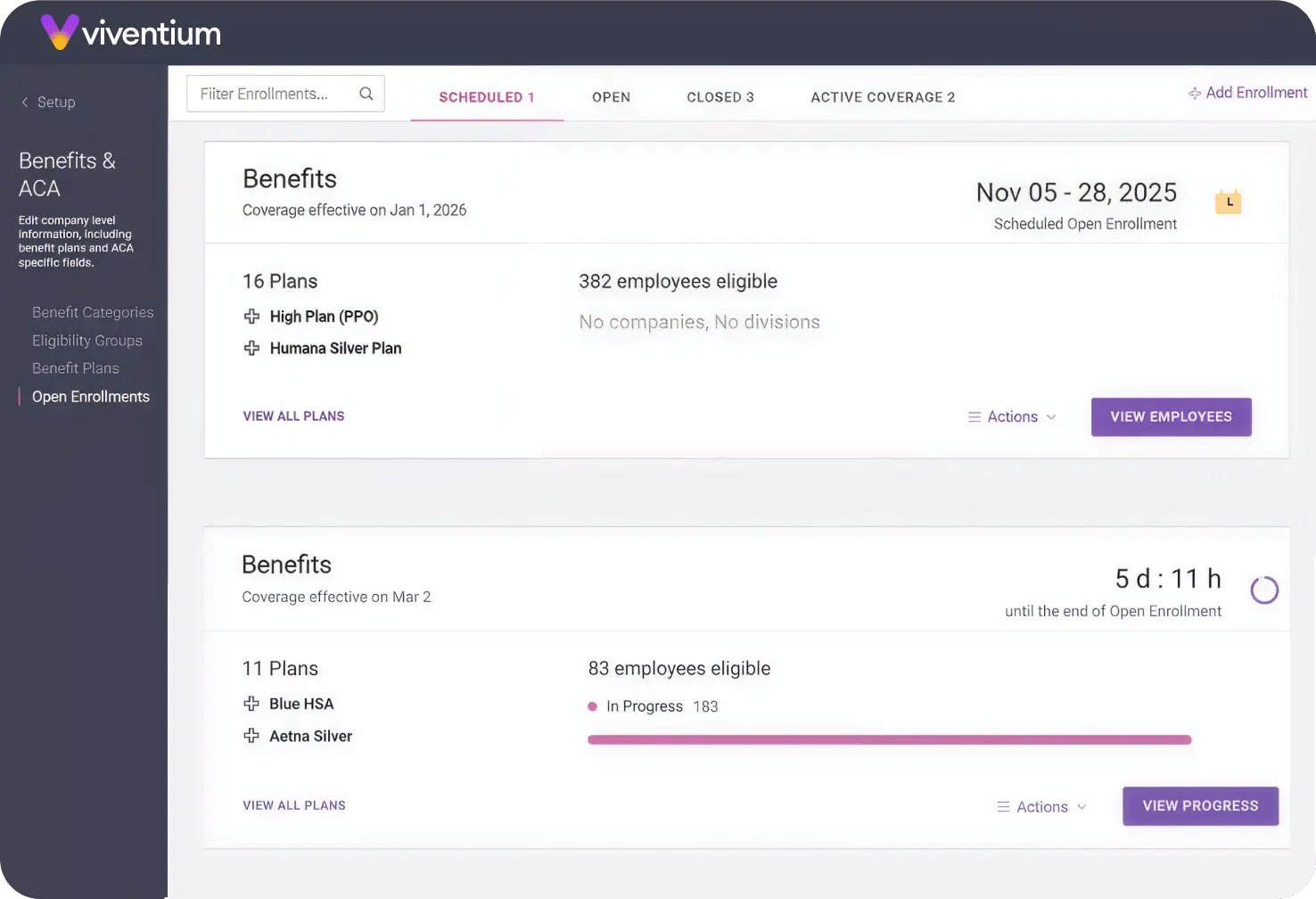
Track employee offers and enrollments
Monitor employees’ offers, enrollments, and waivers to maintain compliance
Penalty exposure alerts
Receive alerts when offers are missing or unaffordable, helping you avoid ACA penalties and stay compliant
Maintain benefit plan information
Keep benefit plan details, employee costs, and essential data to challenge proposed penalties and maintain compliance
Produce year-end ACA forms
Generate and file year-end ACA forms, including Series 1 and 2 codes, electronically with ease
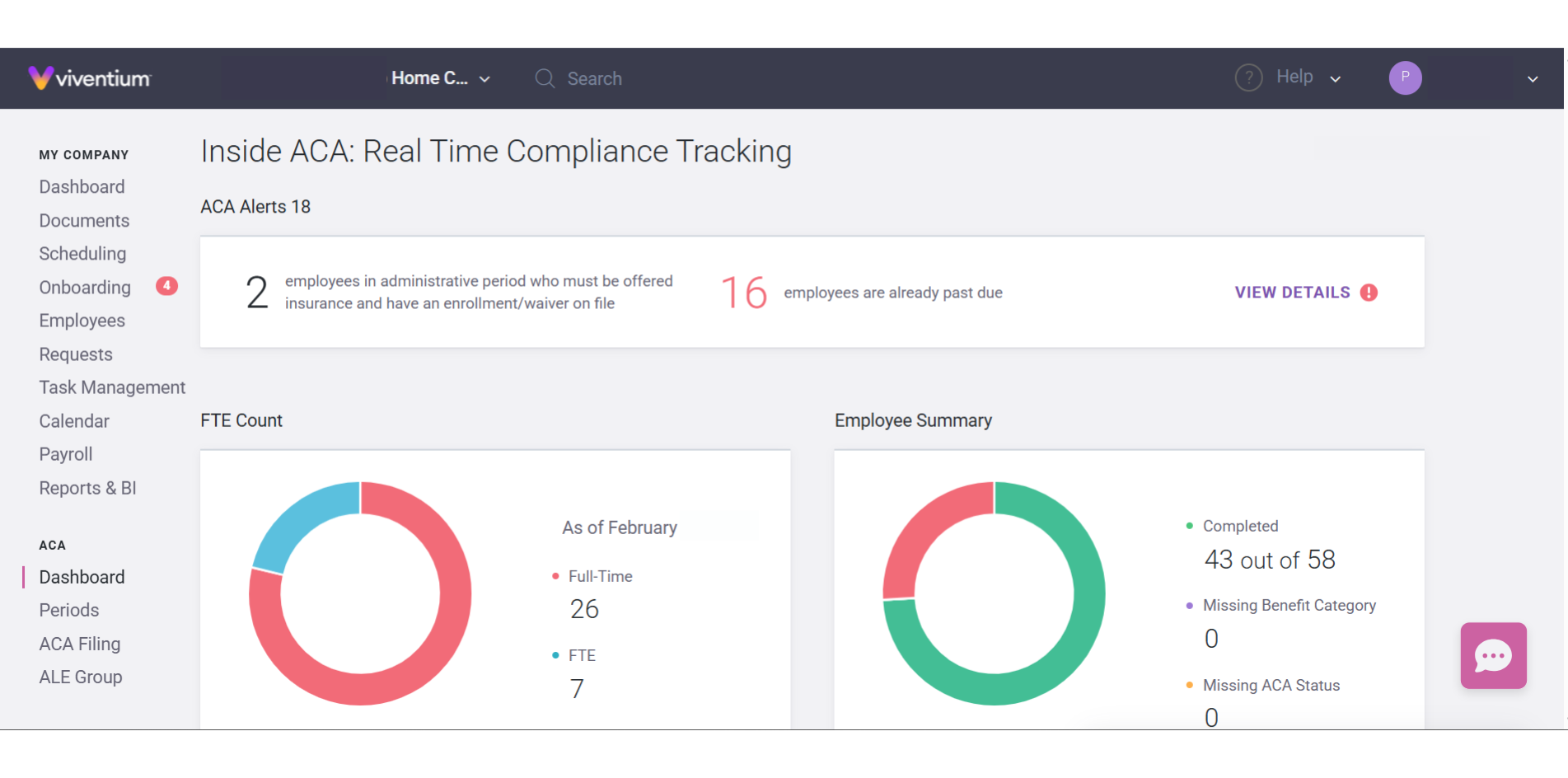
ACA compliance dashboard
Stay compliant by monitoring your ALE status and full-time equivalent (FTE) employee count on a user-friendly dashboard
Visualize compliance data
View your ACA data with a variety of graphical and numerical breakdowns to gain actionable insights
Real-time status updates
Get real-time updates on employees’ full-time and part-time status to ensure accurate reporting
Automatic status change list
Automatically generate a list of employees whose status changes to keep compliance tracking effortless
Amendments
Have a need for an amendment to your previously filed forms? Create, review and file that amendment all within Viventium.
Proven. Trusted. Preferred.
Solutions Tailored to Your Role Lorem
Administrators
Lorem ipsum dolor sit amet consectetur. Vestibulum molestie donec neque pharetra sem porttitor est id pharetra.
CEO
Lorem ipsum dolor sit amet consectetur. Vestibulum molestie donec neque pharetra sem porttitor est id pharetra.
Role/Persona
Lorem ipsum dolor sit amet consectetur. Vestibulum molestie donec neque pharetra sem porttitor est id pharetra.
Role/Persona
Lorem ipsum dolor sit amet consectetur. Vestibulum molestie donec neque pharetra sem porttitor est id pharetra.
"Viventium is a perfect blend of a great product and a great service. The software itself is extremely user-friendly, especially compared to other solutions we’ve tried, and the client service really stands out."

Simon Mord
Big Apple Homecare
Explore our entire product suite
Applicant Tracking
Onboarding

HR

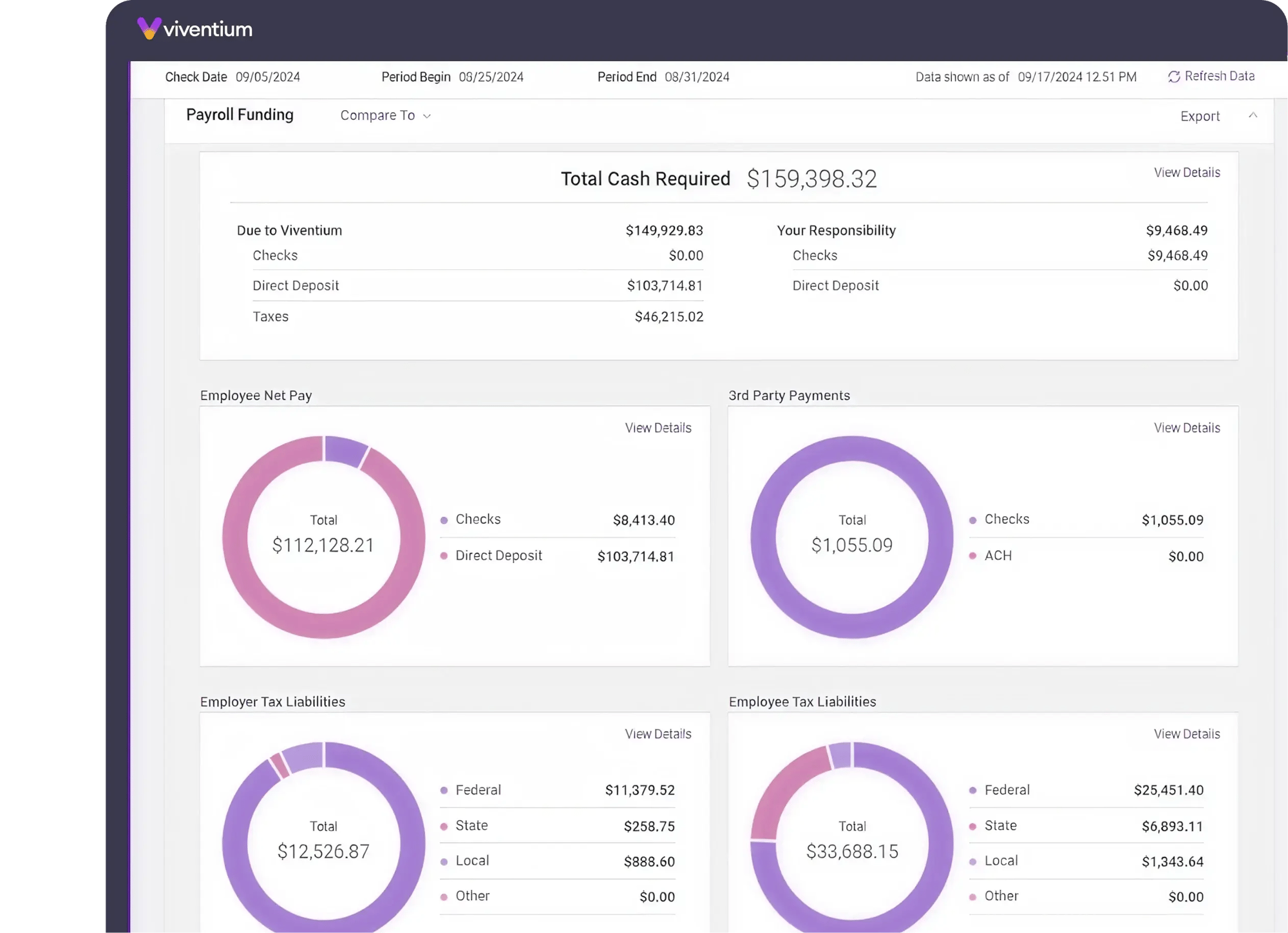
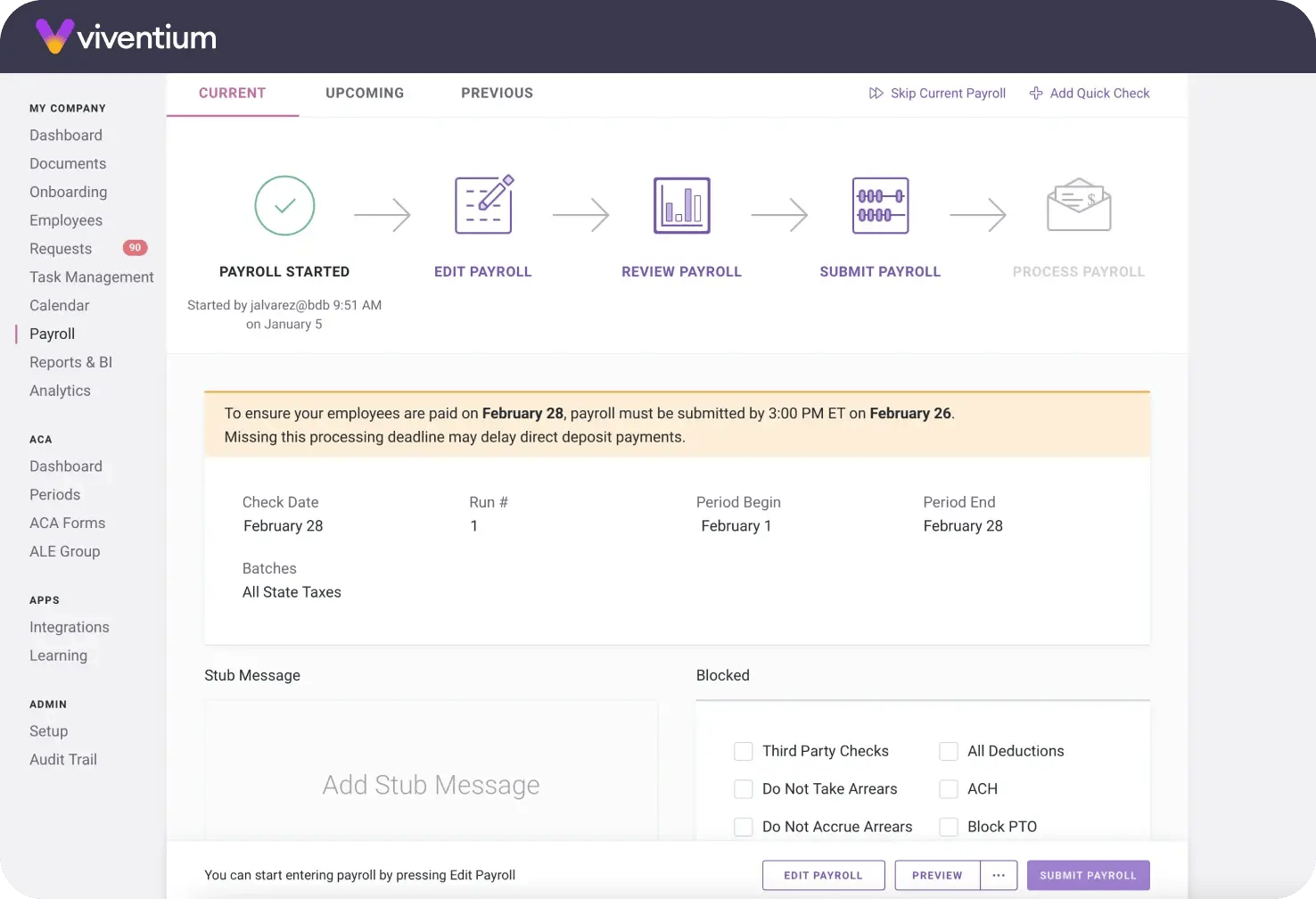
Payroll
Benefits Administration
Scheduling

Time & Attendance

ACA Compliance

Business Intelligence

Learning Management

Expand your HR compliance expertise
Featured Resources

Guide

Skilled Nursing

Blog
Featured Resources



Based on 1,000+ reviews from